- Home
- Why Truffles?
- Blog
- You Can't Run from Vein Disease
- VenaSeal
- Summer is Almost Over
- IDK about Vein Disease
- Vein Treatment Fayetteville
- Sonography to RN Degree Program
- Vein Testing Differences
- Advantage of Vein Treatment Before Knee Surgery
- Poor Medical Advice
- Green Tomatoes for Varicose Veins
- VenaSeal Treatment Atlanta
- Fake News
- Iliac Vein Compression
- Vein Treatment
- DVT
- Pelvic Health
- Sclerotherapy
- leg swelling
- The Vein Specialists
- Vein Treatments
- What is Vein Disease
- Vein Conditions
- Vascular Testing
- Look and Feel Your Best!
- Reviews
- Media
- Contact Us
- Schedule and Appointment
- Free Vein Screening
- Give Us Feedback
- Referral Resources
- Make a Payment
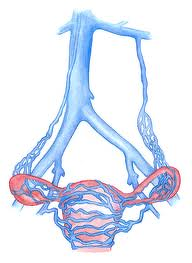
Pelvic Congestion Syndrome
Pelvic congestion syndrome is commonly missed and oftentimes results in unnecessary procedures and testing. Nearly 25% of women who visit an OB/GYN for pelvic pain have pelvic congestion syndrome. Pelvic congestion is caused by varicose veins in and around the pelvic organs. This is often secondary to compression of the iliac vein in the abdomen. Signs and symptoms include pain during or after intercourse, pain in the legs during menstruation, hip pain, low back pain, irritable bowel symptoms, irritable bladder symptoms, labial veins, hemorrhoids, and vein around the outer thigh, posterior thigh and groin area. Vein disease above the waist is not often diagnosed at most vein centers. Brian Sapp, RVT, RPhS is one of the few vascular technologists in the country who performs this kind of testing and teaches the advanced venous course for Philips Healthcare. Truffles Vein Specialists specializes in the diagnosis of all vein disease including pelvic and iliac vein disease.
High pressure and stretching of veins in the pelvis may result in pelvic pain, tenderness, or dyspareunia (pain with intercourse). The pain can be either a dull, aching pain or a sharp, deep pain. This pain often is worse just before menstrual period, with prolonged standing, or with intercourse. Once other pelvic organ pathology such as cysts or abnormal growth of the uterus or ovaries or infection have been ruled out, the syndrome commonly is labeled Pelvic Congestion Syndrome.
Some patients with Pelvic Congestion Syndrome (PCS) have an underlying correctable problem. Some have pelvic (iliac) vein obstruction and others have pelvic varicose veins due to venous blood running in the wrong direction from the upper abdomen toward the pelvis. Ovarian vein blood flow usually goes from the ovary toward the left renal (kidney) vein or toward the inferior vena cava, the large vein in the abdomen carrying blood back to the heart. If the one-way valves in the ovarian vein have failed, blood will flow in a reverse direction (reflux) toward the pelvis. Ovarian vein reflux can cause very high pressures to develop in the veins of the pelvis, sometimes causing pelvic pain, dyspareunia, and varicose veins in the deep pelvis.
A similar process in the male causes reflux of blood down a testicular vein into the scrotum. The high venous pressures in the scrotum result in progressive development of varicose veins in the scrotum and the spermatic cord which connects the testicle to the rest of the body. These scrotal varicose veins are called a varicocele. Some varicoceles cause pain, especially with lifting; others reduce the sperm count and may be responsible for male infertility. Treatment of the varicocele by sealing the testicular vein usually resolves the pain or infertility problem.

Pain during intercourse (dyspareunia) is pain or discomfort in a woman's labial, vaginal, or pelvic areas during or immediately following sexual intercourse. The word dyspareunia comes from the early Greek language, and its meanings include "badly mated" or "difficulty mating". Pain during intercourse is described in medical literature dating back to the ancient Egyptian scrolls. Today, most causes of dyspareunia can be easily discovered and treated.Many women experience some pain during their first episode of vaginal sexual intercourse. In studies 25% of all women who visit the OB/GYN for pelvic pain during intercourse have what is known as pelvic congestion. This should be easy to diagnose, however typical GYN ultrasounds while looking directly at the varicose veins around the uterus do not document the findings. Also, both doctors and women fail to freely discuss sexual practices. Recent studies suggest that more than many women report current or previous episodes of pain during sexual relations. Fewer than half of these women discussed this pain with their doctors.
What Are the Symptoms of Painful Intercourse (Sex)?
Symptoms of pain related to sexual intercourse can occur when entry is attempted or during and/or immediately following sexual intercourse.The most common symptom is pain on entry (intromission). The pain may be described as sharp or burning.The second most common symptom is deep pain. Other symptoms include feelings of muscle spasms, pelvic cramping, or muscle tightness. Pain during intercourse may be described as primary or secondary; as complete or situational; and as superficial-entrance or deep thrust types.
Primary pain with intercourse is pain that has existed for the woman's entire sexual lifetime. Secondary pain develops after a symptom-free period of time. Complete pain means the woman experiences pain in all times during intercourse. Situational pain occurs with a particular partner or a certain type of stimulation. Superficial-entrance pain is noticeable at penetration. Deep thrust pain is located at the cervix or in the lower abdominal area and is noticeable during or after penetration. A woman may perceive pain during intercourse even without any physical cause. Many health professionals believe that sexual pain without an apparent physical cause may have a psychological origin, however new technology and advances in venous imaging have identified pelvic congestion as a cause of 25% of dyspareunia. Recent studies suggest that 60% of women who have been treated with psychological issues have pelvic congestion syndrome. When these women are treated they get better!
Pelvic congestion syndrome (also known as chronic pelvic vein incompetence) is a medical condition caused by the compression of the iliac veins by surrounding structures such as the pelvic bones, abdominal muscles, and ligaments. This compression over time can cause pressure build up in the veins, leading to pain in the pelvic region, heaviness in the pelvic area, painful intercourse, back pain, IBS, irritable bladder and other symptoms. Nutcracker syndrome, another form of pelvic congestion syndrome, is a very specific type of vein compression syndrome that occurs when the left renal vein is compressed between the abdominal aorta and the superior mesenteric artery. Symptoms of nutcracker syndrome include abdominal fullness, flank pain, lower back discomfort and the presence of blood in the urine (microscopic hematuria). Treatment for pelvic congestion syndrome involves treating the underlying pathology, including minimally invasive treatments like varicose vein embolization may be recommended.
